Overcoming Health Disparities – Edgecombe County
Health outcomes vary by racial and ethnic background in North Carolina. Length and quality of life are worse for Native Americans and African Americans. Racial disparities begin early, as African American babies are more than twice as likely to die during childbirth than white or Hispanic babies in North Carolina. Additionally, a Black woman in North Carolina is three times more likely to die from childbirth than a white woman.

The Challenge
Health outcomes vary by racial and ethnic background in North Carolina. Length and quality of life are worse for Native Americans and African Americans. Racial disparities begin early, as African American babies are more than twice as likely to die during childbirth than white or Hispanic babies in North Carolina. Additionally, a Black woman in North Carolina is three times more likely to die from childbirth than a white woman. These disparities also affect common chronic illnesses, like heart disease, diabetes, and cancer rates. A report by Dr. Caroline Ames, a urologist, underscores these health disparities. Dr. Ames found that not only does Edgecombe County have a prostate cancer mortality rate (41.9%) nearly twice the average in NC (23%), but also that low-income African American men are disproportionately affected.
Access to reliable primary care and early detection screenings can dramatically lower the odds of dying from prostate cancer, which is the second-leading cancer death cause in the nation. African Americans suffer a disproportionately high incidence of and mortality from prostate cancer compared to whites, according to this study in the NC Medical Journal. Multiple factors may prevent men, including African American men, from getting tested and treated for prostate cancer. Misconceptions exist about the effects of treatment on men’s bodies, including that prostate screenings are painful and emasculating and that treatment of an enlarged prostate can lead to sexual dysfunction or incontinence. African American men in eastern NC also may experience higher risk factors, including a diet lower in fruits and vegetables and higher in meats and fats, because of food deserts and other systemic food insecurity issues. Finally, access to healthcare in rural North Carolina compounds risks, as those who are un- or underinsured for health insurance, low-income, or have limited transportation are less likely to regularly attend medical appointments and receive necessary cancer screenings.
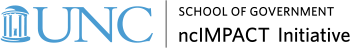
Racial and Ethnic Health Disparities in NC, from the NC Health Equity Report.
The Solution
To address this prostate cancer mortality disparity, Vidant Edgecombe Hospital, the Vidant Multispecialty Clinic, and local barbers in Edgecombe County joined together in the Edgecombe County Barbershop Partnership. The program works to increase prostate cancer awareness in African American men through their local barbers. Vidant Edgecombe Hospital hosts quarterly meetings and continually educates the participating barbers on early detection, screening, access to care, and other resources that they can share with their clients. Additionally, barbers are educated on myths, facts, and conversation-starters so they can best inform their clients.
As trusted members of the community, barbers are able to promote positive norms regarding screening and provide social support to their clients. Brandon Richardson, a barber who participates in the program, says that he has served some of his clients for five or more years, and knows their families, birthdays, and children’s names. He says that these long-standing relationships make it easy to ask what may seem like personal questions about a person’s family history of prostate cancer and other risk factors or symptoms, as well as direct them to resources for care.
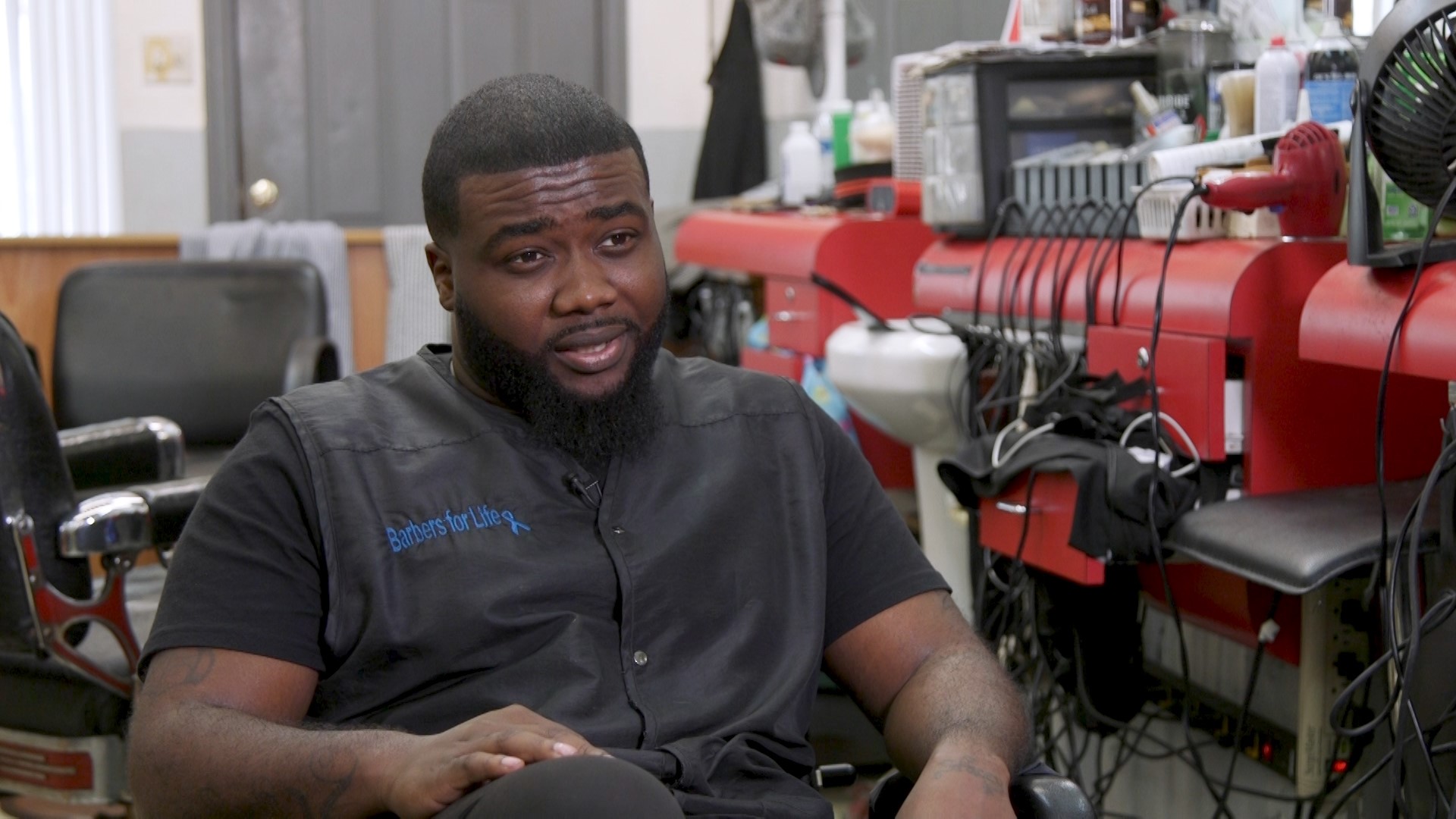
Brandon Richardson, a barber at Master’s Barbershop in Rocky Mount, speaks about his participation in the Edgecombe County Barbershop Partnership.
The Players
This collaborative program is administered by Vidant Edgecombe Hospital and the Vidant Multispecialty Clinic, alongside the ten local barbers in nine shops that educate their clients about screening, access to care, early detection, and myths associated with prostate cancer. The hospital and clinic engage barbers via quarterly meetings and continuing education workshops that keep them informed and supported in their outreach work. Dr. Caroline Ames, who compiled the data on prostate cancer mortality in the county, helped found the program. Its funding comes from MultiPlan, a healthcare management company, who provided a Rural Health Outreach grant to the hospital to fund the partnership.
The Promise
Charles Williams, a prostate cancer survivor, says that when it comes to cancer, “it’s always going to shock you. But this isn’t a game. There’s no replay… you have to take control of your health.” For him, that included regular screenings starting in his 40s, which helped him catch his cancer early and get treatment. Programs like the Edgecombe County Barbershop Partnership lead to increased numbers of men getting reliable information about prostate cancer from trusted sources, including about free early detection testing at Vidant Hospital. As of the 2017 progress report, the barbers educated 533 African American men about prostate cancer testing and treatment. Similar barbershop models are being used in Wilson, NC, Maryland, and Arkansas.
Dr. Ronny Bell, associate director for the Center for Health Disparities at East Carolina University, identified poverty, discrimination, and lack of access to quality healthcare as factors in Edgecombe County and eastern North Carolina. He says collaborative partnerships in smaller communities are key for reducing instances of serious medical conditions like diabetes, stroke, and various cancers. Collaborations provide communities with trusted, local supports and information that can improve participants’ views of healthcare providers and encourage healthy behaviors like prostate cancer screenings. Communities interested in implementing similar programs should look to resources provided by the NC Office of Minority Health and Health Disparities, which created statewide health equity recommendations, as well as to local leaders who can help governments and healthcare providers with community outreach.