The Lack of Rural Healthcare Options Blog
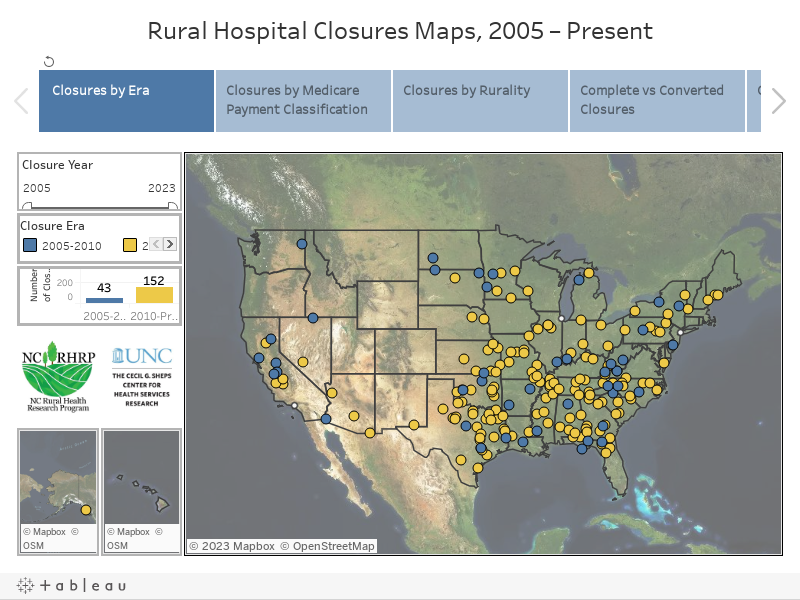
According to the Cecil G. Sheps Center for Health Service Research, North Carolina’s rural communities have faced 152 rural hospital closures and conversions since 2005. The loss of access to healthcare is particularly harmful to those in rural communities who already face health disparities. It makes them more vulnerable to untreated health issues like strokes and heart attacks.

The Problem
The closure of Vidant Pungo Hospital in Belhaven, North Carolina, resulted in a significant adverse impact on the rural community. Former mayor Adam O’Neill led two marches to Washington, D.C, to protest the closure. Others used different strategies, but the hospital ultimately shut down in 2014 due to its poor condition, location in a flood zone, and financial losses. The closure affected communities beyond Belhaven. It created a 130-mile section of North Carolina with no emergency room. This large swath of the state, from Manteo to Washington, was left without proximate access to hospital-level medical care.
Looking past the impact on healthcare, the economic impact on the 1,600-person community was estimated to be around $17 million per year. Over 100 people lost their jobs when the hospital closed in 2014.
According to the Cecil G. Sheps Center for Health Service Research, North Carolina’s rural communities have faced 152 rural hospital closures and conversions since 2005. The loss of access to healthcare is particularly harmful to those in rural communities who already face health disparities. It makes them more vulnerable to untreated health issues like strokes and heart attacks.
The Solution
Two collaboration models have emerged to respond to the lack of healthcare in some rural communities. The first seeks to place more doctors in rural areas. About a decade ago, the UNC Family Medicine Residency program created a rural track to attract doctors who wanted to practice in rural areas. The rural track program is highly competitive and attracts residents with a passion for learning in a community-based setting. The program operates through Piedmont Health Services, the oldest community health center in the state. The organization operates in rural Caswell County, bridging the healthcare cap and meeting the needs of the underserved and under-resourced. The residency program trains doctors to provide care without relying on expensive tests and treatments, as many patients are uninsured and cannot afford such services.
The second model takes healthcare professionals from urban areas to rural areas. For example, the Congregational and Community Nurse Program with Cone Health operates a fleet of vehicles that bring healthcare services to remote areas across Rockingham, Guilford, Alamance, and Randolph counties. This program helps fill gaps in healthcare access for patients who lack access to care, often due to long distances between communities and medical facilities. Trish Gilley, a nurse in the program, is glad to be part of the mobile program, as it allows her to give back to the families with whom she grew up. The program aims to connect patients with any resources they need, ensuring they receive the right care.
The Players
Local churches are partners in the Cone Health program, strengthening community trust and forming a backbone for the program’s success. The program provides screening and acute care services for patients who may need help knowing where to go for healthcare services. This helps address gaps in healthcare access and is important in rural communities where patients do not always have access to the right care or even know they have conditions. Cone Health officials believe that their relationship with local churches will only get stronger, which will help strengthen trust in the community, making it easier to provide healthcare services to their rural communities.
The Family Medicine Residency program benefits both doctors and rural communities, as research shows that those who train in rural areas are more likely to practice in rural areas. The program has become competitive in recent years and has successfully attracted doctors from all over the United States of America. This includes students originally from rural places in North Carolina looking to return and serve communities like the ones in which they grew up. Healthcare leaders say the collaboration between the UNC School of Medicine and community health centers is an ideal model for North Carolina and can be used in rural areas nationwide.
The Promise
Neither of the profiled programs replaces the proximity benefit for rural communities that have lost their hospital. However, both demonstrate creativity in ensuring rural residents have access to primary and acute care that may save them a trip to the hospital later.